End-effectors at mm scale
 The small scale of minimally-invasive surgical procedures presents significant challenges to developing robust, smart, and dexterous tools and end-effectors for manipulating millimeter and sub-millimeter anatomical structures (e.g. vessels or nerves) and surgical equipment (e.g. sutures or staples). To meet the demand, we are developing a versatile fabrication process, based on printed circuit board manufacturing techniques, to create monolithic, kinematically complex, three-dimensional machines in parallel at the millimeter to centimeter scales. During lamination, precisely aligned material layers are combined in different ways to create functional layers that serve a specific purpose, including structural layers, flexure layers that enable rotary joints and articulated structures, printed circuit board (PCB) layers, metal spring layers, or low-friction sliding bearing layers. Finally, various functional layers combine to create multi-structure, multi-material, quasi-2D laminates capable of folding into complex 3D structures.
The small scale of minimally-invasive surgical procedures presents significant challenges to developing robust, smart, and dexterous tools and end-effectors for manipulating millimeter and sub-millimeter anatomical structures (e.g. vessels or nerves) and surgical equipment (e.g. sutures or staples). To meet the demand, we are developing a versatile fabrication process, based on printed circuit board manufacturing techniques, to create monolithic, kinematically complex, three-dimensional machines in parallel at the millimeter to centimeter scales. During lamination, precisely aligned material layers are combined in different ways to create functional layers that serve a specific purpose, including structural layers, flexure layers that enable rotary joints and articulated structures, printed circuit board (PCB) layers, metal spring layers, or low-friction sliding bearing layers. Finally, various functional layers combine to create multi-structure, multi-material, quasi-2D laminates capable of folding into complex 3D structures.
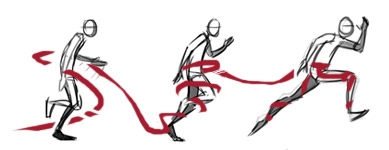
Assured safety drill
We have developed an assured safety drilling mechanism that is compatible with a large range of bit diameters and provides safe, reliable access to the inside of the skull. This is accomplished through a dynamic bi-stable linkage that supports drilling when force is applied against the skull but retracts upon penetration when the reaction force is diminished. In the initial design retraction was achieved when centrifugal forces from rotating masses overpower the axial forces, thus changing the state of the bi-stable mechanism. The current design iteration features a torsional spring loaded mechanism that overpowers axial forces upon penetration, thus triggering the change in the bi-stable mechanism. Testing on ex-vivo animal structures has demonstrated that the device can withdraw the drill bit in sufficient time to eliminate the risk of soft tissue damage. Ease of use and portability of the device will enable its use in unregulated environments such as hospital emergency rooms and emergency disaster relief areas.